
Lupine Publishers Group
Lupine Publishers
Menu
ISSN: 2637-4544
Research Article(ISSN: 2637-4544) 
Pain Management in Outpatient Intrauterine Device Placement and Hysteroscopy: A Survey of Current Practices Volume 4 - Issue 3
Mariana Sucena1, Maria Malheiro2, Fernanda Águas1, Margarida Martinho2, Daniel Pereira da Silva3*
- 1Department of Obstetrics and Gynecology, Coimbra Hospital and University Centre, Praceta Professor Mota Pinto, Portugal
- 2Department of Gynecology, São João Hospital and University Centre of Porto, Alameda Professor Hernâni Monteiro, Portugal
- 3Coimbra Medical Institute, Coimbra, Portugal
Received: April 13, 2021Published: April 27, 2021
Corresponding author: Daniel Pereira da Silva, Coimbra Medical Institute, Rua do Brasil 133, 3000 Coimbra, Portugal, Email:dpdaSilva@sapo.pt
DOI: 10.32474/IGWHC.2021.04.000193
Abstract
Objective: To survey obstetricians and gynecologists routine pain control practices in office intrauterine device insertion and hysteroscopies.
Methods: An observational cross-sectional survey-based study was conducted to evaluate the current pain management practices in outpatient gynecological procedures in Portugal. Type of protocols applied and their frequency as well as the possibility of using an alternative local strategy were addressed.
Results: Of the surveyed professionals, 198 (49.5%) implemented pain reduction protocols when inserting intrauterine devices. Non-steroid anti-inflammatory drugs (49.5%) were the first choice followed by the use of misoprostol (22.7%). Respondents reported a higher percentage of pain management during hysteroscopy (87.4%), opting mostly for general anesthesia. More than 85% of the ob-gyn would adopt a local anesthetic solution developed specifically for this purpose, highlighting that the current applied methodologies are frequently ineffective.
Conclusion: Current pain control methods for office procedures are not totally effective and are a major limiting factor. More efficient pain control methods and guidelines are needed for gynecological procedures in an office setting. birth weight is detected early and treated appropriately. They should be followed up to ensure normal progression of pregnancy.
Keywords: Pain Management; Intrauterine Devices; Hysteroscopy; Office Setting; Anesthetics
Introduction
Gynecological procedures are common in women regardless of their age [1]. When compared to interventions performed in the operating room under general anesthesia, an office setting diminishes the risks of anesthesia complications and hospitalization, while minimizing recovery time, as well as the need for equipment and associated costs [2]. Insertion of intrauterine devices (IUDs) and hysteroscopies in an office setting have increased significantly in recent years [3]. These are minimally invasive and safe procedures and, thus associated with tolerable pain and discomfort [4]. Furthermore, they are regularly performed without analgesia or anesthesia, devaluing the anxiety and pain reported by women [5]. Pain experienced by women is quite often classified as “moderate” or “severe”, leading to the interruption of the gynecological procedure [5,6]. A noteworthy study conducted on 417 patients concluded that 12.4% of women reported “hardly tolerable” pain and 3.6% reported “intolerable” pain when undergoing hysteroscopy without anesthesia or analgesia [7]. When inserting IUDs, the prevalence of reported “moderate” to “severe” pain ranges from 11% to 47% [8,9]. In nulliparous women, these numbers can be even more severe with 80% of women reporting moderate to severe pain [10]. Therefore, effective strategies for pain relief are of particular relevance. Different analgesia and anesthesia methods such as oral, intramuscular and intravenous medication and paracervical block have been described for pain relief in gynecological procedures [5,6]. A recent systematic review concluded that the administration of oral non-steroids anti-inflammatory drugs (NSAIDs) before, during and after hysteroscopy significantly reduces pain [11]. In contrast, a Cochrane review revealed insufficient evidence of a clinically significant effect when different types of analgesia were compared in women undergoing ambulatory hysteroscopy [12].
A similar scenario is described in pain management associated with IUDs insertion where limited efficacy of local anesthesia (2% lidocaine gel), misoprostol and oral administration of NSAIDs is reported [13]. Scientific data is inconsistent in demonstrating the existence of a highly effective strategy to control pain and discomfort associated with gynecological procedures and the superiority of one strategy over the others [3,12]. According to guideline no. 11/DSCS/DPCD of June 18, 2008, issued by the Portuguese National Health Authority, pain control should be seen as a priority and a criterion for high quality health care [14]. As a result, the development of new methods and the definition of clear guidance for pain control should be a priority. In this study, the practices of obstetricians and gynecologists (ob-gyn) regarding the use of pain control strategies were evaluated in Portugal. The type of protocols used for control of pain and discomfort and the frequency of their use when performing gynecological procedures such as IUD insertions and hysteroscopies were assessed. Effective pain control for women undergoing office gynecologic procedures is critical for both patient comfort and procedure success. Thus, knowledge of clinical practices is essential to establish the need for clinical guidelines. They can lead to more consistent practices, aiming to improve patient tolerance and to increase satisfaction associated to office gynecological procedures with intra-uterine manipulation, especially IUD insertion and hysteroscopy.
Methods
Study Design and Participants
An observational cross-sectional survey-based study was performed during 2020. A questionnaire was created to assess routine clinical practices for pain management in outpatient gynecological procedures. This questionnaire consisted of 14 closeended questions divided into two similar sections, one focused on IUD insertion practices and the other on hysteroscopies. The study was reviewed and exempt from ethical approval by the Clinical Studies Nucleus of the Portuguese Society of Gynecology. Ob-gyn’s participation and completion of the survey was voluntary and completely anonymous. Four hundred and eighty-seven out of a total of 1186 ob-gyn were randomly chosen and invited to complete the questionnaire in a face-to-face model. Fifty-one (10.5%) clinicians did not answer the survey. A total of 436 responses representing the main geographical regions of Portugal, North (n=207), Center (n=70), South and Islands (n=159) were analyzed.
Study Variables
The questionnaire was composed of two parts. The first part was designed to understand pain control practices for IUD insertion and the second part assessed the same aspects regarding performing hysteroscopies. Health professionals were asked about their experience with placement of IUDs and performing hysteroscopies, as well as the type and frequency of pain management strategies used in their routine clinical practice. The possibility of adopting a new local anesthesia strategy design was also assessed.
Statistical Analysis
Data collected from the questionnaires were cleaned and coded. These data were introduced to SPSS Statistics for Windows, Version 21.0 (Armonk, NY: IBM Corporation) for analysis of summary statistics, such as proportions, arithmetic means and 95% confidence intervals. When appropriate, the bilateral Pearson’s Chi- Square test was used and performed at a 0.05 significance level. No adjustments were made for multiple comparisons.
Results
Four hundred and thirty-six ob-gyn answered a questionnaire about their routine practices in controlling pain when inserting IUDs and performing hysteroscopies.
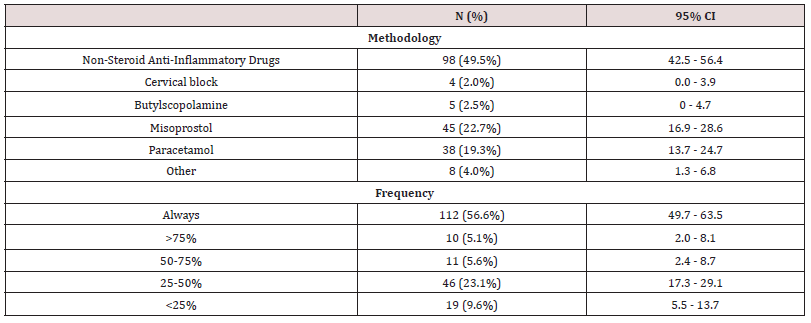
Table 1: Pain management strategies for intrauterine device insertion. The insertion of cooper or levonorgestrel IUDs was performed by 400 (91.7%) of the 436 surveyed physicians and 198 out of the 400 (49.5%) respondents use some type of pharmacological or non-pharmacological intervention to manage pain and discomfort related to IUD placement. One hundred and fifty-nine out of the 400 (87.4%) participants use a pain management and/or discomfort method.
IUD insertion
The insertion of cooper or levonorgestrel IUDs was performed by 400 (91.7%) of the surveyed physicians in their current clinical practice. On average, 314 (78.5%) place one to five devices per month, 59 (14.7%) six to ten and only 27 (6.8%) inserted more than ten IUDs a month. It is noteworthy that only 198 (49.5%) of the respondents use some type of pharmacological or nonpharmacological intervention to manage pain and discomfort related to IUD placement. Among those who implement pain relief strategies, 98 (49.5%) recommend oral NSAIDs, 45 (22.7%) prescribe misoprostol and 38 (19.3%) paracetamols. Only 4, a residual proportion of respondents use paracervical block (2%), 5 use butylscopolamine (2.5%) or 8, other pain control (4%), either pharmacological or non-pharmacological interventions, during IUD insertion [Table 1]. Relevant data are that 112 (56.6%) out of the 198 physicians always use a pain control method and 374 (93.5%) of them would consider using a new local anesthetic solution designed for IUD placement. Of the 26 (6.5%) respondents who would not adopt a local anesthetic solution, 18 (69.2%) do not use any strategy for pain control, 4 (11.5%) use NSAIDs, 3 (15.4%) misoprostol and 1 (3.8%) paracetamol. Of the 202 (50.5%) obgyn who do not use any form of pain control, only 18 (9%) would maintain their position if a new alternative method were offered.
Hysteroscopies
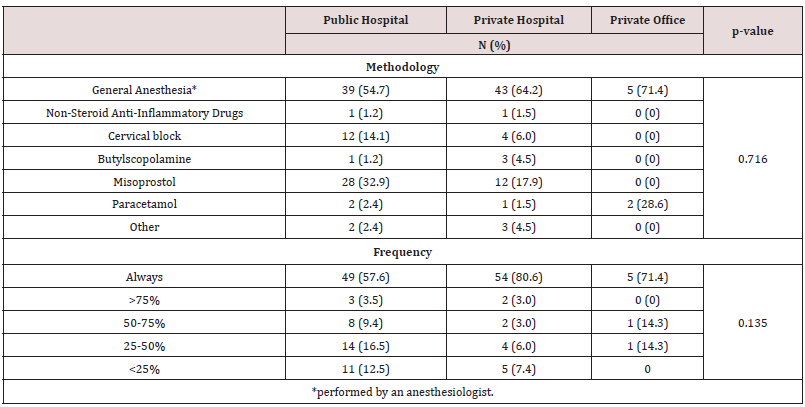
One hundred and eighty-two (41.7%) of the ob-gyn who participated in the study perform hysteroscopies and minor surgical hysteroscopic procedures in their clinical practice. Most of the participants, 98, perform them in a public hospital (53.8%), 70 (38.5%) in a private hospital and 14 (7.7%) in their private office. Approximately half of the participants, 89, (48.9%) perform one to five hysteroscopy procedures by month, 51 (28.0%) six to ten and 42 (23.1%) complete more than 10 hysteroscopies a month. One hundred and fifty-nine (87.4%) of the participants use a pain management and/or discomfort method. Remarkably, 87 (54.7%) ob-gyns opted to perform hysteroscopies in ambulatory setting, resorting to general anesthesia carry out by an anesthesiologist. Misoprostol was recommended by 42 (26.4%) clinicians and cervical block was performed by 16 (10.1%) in office hysteroscopies. One hundred and eight (67.9%) participants report having always used a pain control strategy [Table 2]. The pattern of pain control strategy and frequency of use was not correlated with the healthcare sector where hysteroscopies were performed (p=0.716) [Table 3].
Table 2: Pain control methodologies applied during hysteroscopies. One hundred and eighty-two out of the 436 (41.7%) ob-gyn who participated in the study perform hysteroscopies and minor surgical hysteroscopic procedures in their clinical practice.
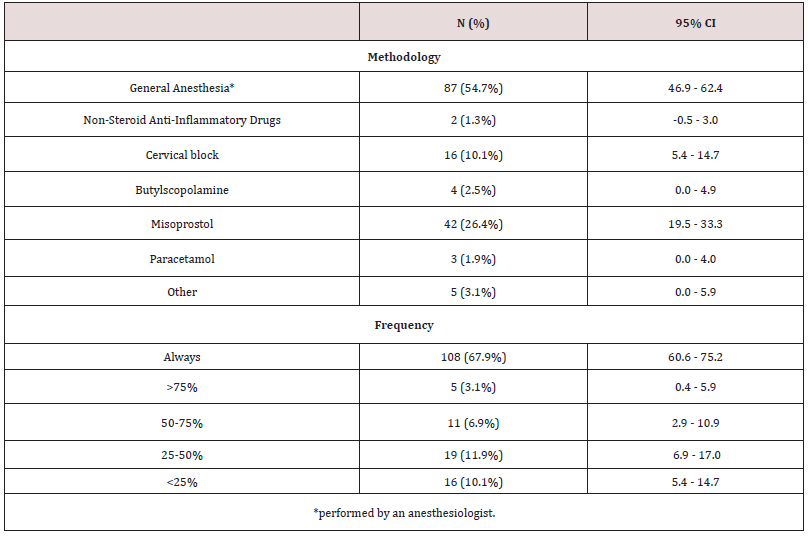
Table 3: Comparison between the type and frequency of pain control techniques used in hysteroscopies, according to health care sector. From the 182 (41.7%) ob-gyn who perform hysteroscopies and minor surgical hysteroscopic procedures in their clinical practice, 98 perform them in a public hospital (53.8%), 70 (38.5%) in a private hospital and 14 (7.7%) in their private office. Globally, 195 (87.4%) of the participants use a pain management and/or discomfort method.
Most clinicians, 155 (85.2%), would consider using a local anesthetic solution designed for hysteroscopic procedures. Of the 27 (14.8%) respondents who would not adopt an alternative local anesthetic solution, 36 (96.3%) used general anesthesia as a method of pain control.
Discussion
A relevant percentage of women would benefit from pain management interventions in outpatient gynecological procedures, although they can be performed without anesthesia or analgesia, particularly in an office setting [15]. Different pain and discomfort management strategies such as oral medication (NSAIDs and misoprostol), local anesthesia, and intravenous anesthesia are used for gynecological procedures [16,17]. In spite of these possibilities, controversy exists about which the more appropriate strategy is to use as high-quality evidence is lacking. The absence of guidelines also leads to heterogeneous clinical practice with most of clinicians not resorting to any pain control strategy, potentially impacting women’s experiences and thus quality of life.
Our study shows the heterogenicity of pain control protocols used both for the insertion of IUDs and outpatient hysteroscopies, in line with other studies [1-19]. The most tested methods reported in the literature for controlling pain when inserting IUDs are oral NSAIDs and misoprostol and both topical and injected lidocaine [20]. However, scientific evidence is inconsistent on the benefit of these pharmacological interventions in controlling pain [13]. In fact, only some of the lidocaine formulations, the opioid tramadol and the NSAIDs naproxen have exhibited a modest effect in pain relief [13].
Our study showed that the use of NSAIDs, administered either orally or intramuscularly, is the most common practice for controlling pain when inserting IUDs. In fact, this approach is reported transversally in the literature with the aim of improving tolerance during and after the procedure. However, several studies have shown a lack of benefit from ibuprofen for the insertion procedure itself [21,22]. Paracetamol used by 19.3% of participants is inferior to ibuprofen for pelvic pain with uterine origin, but it is a safe option when NSAIDs are contraindicated [23]. With regard to hysteroscopy procedures, pain remains the main limiting factor for wider use in an office setting. The number of ob-gyns who implemented an analgesia strategy was higher in the present study when compared to other studies, where only 34 to 38% of respondents had analgesia strategy in place [18,19]. General anesthesia, despite requiring more demanding patient monitoring and its association with potentially greater perioperative complications, was the predominant physician choice for performing hysteroscopies in an outpatient setting, similar to the outcome of a study carried out in 2009 [24]. Likewise, the use of different pain control protocols is similar to other published studies [18-25]. Misoprostol was the second most used strategy in both procedures. Data demonstrate that its use reduces cervical resistance and the need for cervical dilatation in pre-menopausal women [26,27]. Thus, it would be expected to have a positive impact on pain and tolerance to these procedures. Yet, different studies have shown that misoprostol does not facilitate IUD insertion and, in addition, it leads to an increase in side effects such as nausea, vomiting, fever, pain and bleeding [28- 31]. Similarly, data do not support its systematic use for improving tolerance to hysteroscopies in an office setting [32].
The prescription of antispasmodics such as butylscopolamine was very reduced in both procedures analyzed in this study. In fact, the use of these substances is related to an increase in adverse effects including nausea, dizziness, fatigue and gastrointestinal disturbances [11]. Likewise, the performance of cervical block was also residual among ob-gyn included in this study. Although cervical block has been shown to be effective for many gynecological procedures, the puncture itself causes considerable discomfort. In addition, the potential occurrence of serious complications must be considered. Accidental intravasation leading to cardiovascular impairment by systemic vasodilation and effects on the central nervous system have been reported [33,34].
In recent years, “hysteroscopic anesthesia” has emerged as a promising and effective local anesthesia technique [35,36]. It consists of the injection of 1% lidocaine under hysteroscopic guidance directly at the site of the intra-uterine lesion using an endoscopic needle only when requested by the patient [37]. Nevertheless, all local anesthetic techniques carry the risk of complications related to intra-vascular injection [33] and due to the technical challenge they pose, they should be reserved for selected cases and performed by experienced professionals in a hospital environment. Most analgesia regimens and local anesthesia techniques have been adapted from other medical procedures and, therefore, their effectiveness in relieving pain associated with gynecological procedures has not been consistently demonstrated [12,13]. This is recognized by the American College of Obstetricians and Gynecologists and by the Royal College of Obstetricians and Gynecologists and reinforces the need for alternative forms of pain management [3-39]. The responses of ob-gyns who participated in this study also corroborated this as the great majority of them would consider using a new form of local anesthetic. To the best of our knowledge, this study is the first known research in Portugal assessing pain relief strategies used by ob-gyns during their clinical practice in outpatient procedures such as the insertion of IUDs and hysteroscopies. Nevertheless, this study has some limitations. Although this is a national study based on 436 questionnaires, the recruited physicians had previously consented to be included in a specific database which may have introduced selection bias. Furthermore, the questionnaire had never been applied before and therefore, validated. However, we have no reason to believe that these limitations would impose on its clinical relevance.
List of Abbreviations:
Ob-gyn: obstetricians and gynecologists, IUD: intrauterine device, NSAIDs; non-steroids anti-inflammatory drugs.
Conclusion
This study concludes that the adoption of pain control strategies is not yet a routine practice when gynecological procedures that involve intrauterine access and manipulation are performed in Portugal. Use of NSAIDs was the preferred method for the insertion of IUDs in office setting. By contrast, hysteroscopies were mainly performed in outpatient care under general anesthesia. Still, the methods used to manage pain vary among health care professionals. The availability and willingness of ob-gyns in the study to use a local anesthetic solution developed specifically for gynecological procedures demonstrate that current strategies for pain and discomfort management are not as effective as clinicians expect. Further investigation and developments in this field should be fostered as well as the definition of clear guidelines for pain management in office gynecological procedures.
Acknowledgments
The authors would like to thank to their colleagues for participating in this study. Data collection, statistical and editorial support were performed by an independent committee, with funding from Gedeon Richter Plc.
Conflict of interest statement
Daniel Pereira da Silva is a Medical Advisor of Gedeon Richter Portugal. The remaining authors have no conflict of interest in relation to this article to disclose.
References
- Ireland LD, Allen RH (2016) Pain management for gynecologic procedures in the office. Obstet Gynecol Surv 71(2): 89-98.
- Urman RD, Punwani N, Bombaugh M, Shapiro FE (2013) Safety considerations for office-based obstetric and gynecologic procedures. Rev Obstet Gynecol 6(1): 8-14.
- (2016) American College of Obstetricians and Gynecologists. Clinical challenges of long-acting reversible contraceptive methods. Obstet Gynecol 128: 69-77.
- Wortman M (2012) Pain Management for Office-Based Surgery: Expanding Our Flight Envelope. J Minim Invasive Gynecol 19(2): 143-145.
- Paulo AAS, Solheiro MHR, Paulo COS, Afreixo VMA (2016) What proportion of women refers moderate to severe pain during office hysteroscopy with a mini-hysteroscope? A systematic review and meta-analysis. Arch Gynecol Obstet 293(1): 37-46.
- Toledano RD, Kodali BS, Camann WR (2009) Anesthesia drugs in the obstetric and gynecologic practice. Rev Obstet Gynecol 2(2): 93-100.
- Bradley LD, Widrich T (1995) State-of-the-art flexible hysteroscopy for office gynecologic evaluation. Am Assoc Gynecol Laparosc 2(3): 263-267.
- Carr SL, Singh RH, Sussman AL, Rogers RG, Pereda B, et al. (2018) Women’s experiences with immediate postpartum intrauterine device insertion: a mixed-methods study. Contraception 97(3): 219-226.
- Dina B, Peipert LJ, Zhao Q, Peipert JF (2018) Anticipated pain as a predictor of discomfort with intrauterine device placement. Am J Obstet Gynecol 218(2): 236.
- Callahan DG, Garabedian LF, Harney KF, DiVasta AD (2019) Will it Hurt? The Intrauterine Device Insertion Experience and Long-Term Acceptability Among Adolescents and Young Women. J Pediatr Adolesc Gynecol 32(6): 615-621.
- De Silva PM, Mahmud A, Smith PP, Clark TJ (2020) Analgesia for Office Hysteroscopy: A Systematic Review and Meta-analysis. J Minim Invasive Gynecol 27(5): 1034-1047.
- Ahmad G, Saluja S, O Flynn H, Sorrentino A, Leach D, et al. (2017) Pain relief for outpatient hysteroscopy. Cochrane Database Syst Rev 10: CD007710.
- Lopez LM, Bernholc A, Zeng Y, Allen RH, Bartz D, et al. (2015) Interventions for pain with intrauterine device insertion. Cochrane Database Syst Rev 29(7): CD007373.
- Direção Geral de Saúde (2008) Circular Normative no11/DSCS/DPCD.
- Gemzell Danielsson K, Mansour D, Fiala C, Kaunitz AM, Bahamondes L (2013) Management of pain associated with the insertion of intrauterine contraceptives. Hum Reprod Update 19(4): 419-427.
- Munro A, Sjaus A, George RB (2018) Anesthesia and analgesia for gynecological surgery. Curr Opin Anaesthesiol 31(3): 274-279.
- Bachi A, Thiagamoorthy G (2020) Analgesia for outpatient gynaecological procedures. Case Reports Women’s Heal 28: e00245.
- Abis P, Bigozzi MA, Dotto J, Petriglia C, Neri M, et al. (2020) Pain Management During Office Hysteroscopy: A Survey of Hysteroscopists. Surg Technol Int 37:161-166.
- O Flynn H, Murphy LL, Ahmad G, Watson AJS (2011) Pain relief in outpatient hysteroscopy: a survey of current UK clinical practice. Eur J Obstet Gynecol Reprod Biol 154(1): 9-15.
- Zapata LB, Jatlaoui TC, Marchbanks PA, Curtis KM (2016) Medications to ease intrauterine device insertion: a systematic review HHS Public Access. Contraception 94(6): 739-759.
- Bednarek PH, Creinin MD, Reeves MF, Cwiak C, Espey E, et al. (2015) Prophylactic ibuprofen does not improve pain with IUD insertion: A randomized trial. Contraception 91(3): 193-197.
- Hubacher D, Reyes V, Lillo S, Zepeda A, Chen PL, et al. (2006) Pain from copper intrauterine device insertion: Randomized trial of prophylactic ibuprofen. Am J Obstet Gynecol 195(5): 1272-1277.
- Marjoribanks J, Ayeleke RO, Farquhar C, Proctor M (2015) Nonsteroidal anti-inflammatory drugs for dysmenorrhoea. Cochrane Database Syst Rev 2015(7): CD001751.
- Tawfeek S, Scott P (2010) National inpatient diagnostic hysteroscopy survey. Gynecol Surg 7(1): 53-59.
- van Wessel S, Hamerlynck T, Schoot B, Weyers S (2018) Hysteroscopy in the Netherlands and Flanders: A survey amongst practicing gynaecologists. Eur J Obstet Gynecol Reprod Biol 223: 85-92.
- Crane JMG, Healey S (2006) Use of Misoprostol Before Hysteroscopy: A Systematic Review. J Obstet Gynaecol Canada 28(5): 373-379.
- Choksuchat C, Cheewadhanaraks S, Getpook C, Wootipoom V, Dhanavoravibul K (2006) Misoprostol for cervical ripening in non-pregnant women: A randomized double-blind controlled trial of oral versus vaginal regimens. Hum Reprod 21(8): 2167-2170.
- Waddington A, Reid R (2012) More Harm Than Good: The Lack of Evidence for Administering Misoprostol Prior to IUD Insertion. J Obs Gynaecol Can 34(12): 1177-1179.
- Bahamondes L, Mansour D, Fiala C, Kaunitz AM, Gemzell Danielsson K (2014) Practical advice for avoidance of pain associated with insertion of intrauterine contraceptives. J Fam Plan Reprod Heal Care 40(1): 54-60.
- Gemzell Danielsson K, Jensen JT, Monteiro I, Peers T, Rodriguez M, et al. (2019) Interventions for the prevention of pain associated with the placement of intrauterine contraceptives: An updated review. Acta Obstet Gynecol Scand 98(12): 1500-1513.
- Mansy AA (2018) Does sublingual misoprostol reduce pain and facilitate IUD insertion in women with no previous vaginal delivery? A randomized controlled trial. Middle East Fertil Soc J 23(1): 72-76.
- Marret H, Simon E, Beucher G, Dreyfus M, Gaudineau A, et al. (2015) Overview and expert assessment of off-label use of misoprostol in obstetrics and gynaecology: Review and report by the Collège national des gynécologues obstétriciens français. Eur J Obstet Gynecol Reprod Biol 187: 80-84.
- El Boghdadly K, Pawa A, Chin KJ (2018) Local anesthetic systemic toxicity: Current perspectives. Local Reg Anesth 11: 35-44.
- Mody SK, Farala JP, Jimenez B, Nishikawa M, Ngo LL (2018) Paracervical block for intrauterine device placement among nulliparous women: A randomized controlled trial. Obstet Gynecol 132(3): 575-582.
- Mairos J, Di Martino P (2016) Office Hysteroscopy. An operative gold standard technique and an important contribution to Patient Safety. Gynecol Surg 13(2): 111-114.
- Paulo A, Mairos J, Martino P Di, Solheiro H, Afreixo V (2015) Office hysteroscopy and pain control, a multicenter comparison by scope size and introducing a novel “hysteroscopic anesthesia” technique. Clin Obstet Gynecol Reprod Med 1(4): 99-103.
- Vinagre C, Mairos J, Martino P Di (2013) Hysteroscopic anesthesia: a new method of anesthesia in ambulatory hysteroscopy. Acta Obs Ginecol Port 7(4): 274-277.
- Opinion C (2020) The use of Hysteroscopy for the Diagnosis and Treatment of Intrauterine Pathology. Am Coll Obstet Gynecol 800. Obstet Gynecol 135(3): 138-148.
- Royal College of Obstetricians and Gynaecologist, British Society of Gynecologists Endoscopists. Best Practice in Outpatient Hysteroscopy (Green-top guideline no58). 2011.

Top Editors
-

Mark E Smith
Bio chemistry
University of Texas Medical Branch, USA -

Lawrence A Presley
Department of Criminal Justice
Liberty University, USA -

Thomas W Miller
Department of Psychiatry
University of Kentucky, USA -

Gjumrakch Aliev
Department of Medicine
Gally International Biomedical Research & Consulting LLC, USA -

Christopher Bryant
Department of Urbanisation and Agricultural
Montreal university, USA -

Robert William Frare
Oral & Maxillofacial Pathology
New York University, USA -

Rudolph Modesto Navari
Gastroenterology and Hepatology
University of Alabama, UK -

Andrew Hague
Department of Medicine
Universities of Bradford, UK -

George Gregory Buttigieg
Maltese College of Obstetrics and Gynaecology, Europe -

Chen-Hsiung Yeh
Oncology
Circulogene Theranostics, England -
.png)
Emilio Bucio-Carrillo
Radiation Chemistry
National University of Mexico, USA -
.jpg)
Casey J Grenier
Analytical Chemistry
Wentworth Institute of Technology, USA -
Hany Atalah
Minimally Invasive Surgery
Mercer University school of Medicine, USA -

Abu-Hussein Muhamad
Pediatric Dentistry
University of Athens , Greece

The annual scholar awards from Lupine Publishers honor a selected number Read More...





